At the beginning of Surviving Schizophrenia: A Manual for Families, Patients, and Providers
To that end, Dr. Torrey offers us a glimpse into the inner experience of people with schizophrenia, in their own words, highlighting the changes that occur as a result of the illness:
- Alterations of the senses
- The most common change, especially early in the course of illness, is heightening of the senses, which become overacute
- "noises all seem louder to me than they were before....it makes it difficult to keep your mind on something when there's so much going on that you can't help listening to."
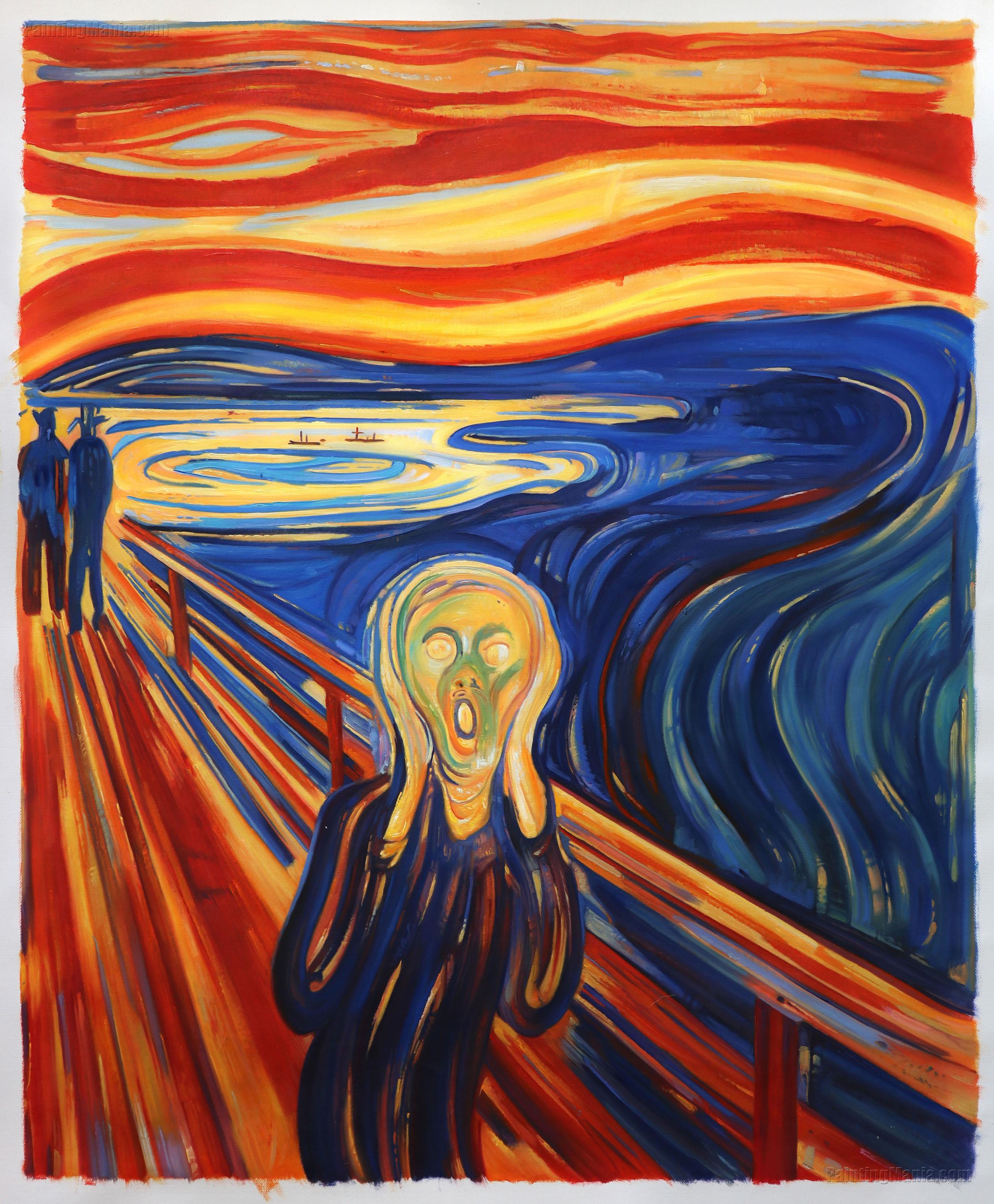
- "Colors seem to be brighter now, almost as if they are luminous painting. I'm not sure if things are solid until I touch them."
- As a result of heightened senses, the person may experience their senses as being flooded with stimuli
- "Sometimes when people speak to me my head is overloaded. It's too much to hold at once."
- Stimuli may become distorted
- "suddenly the room became enormous, illuminated by a dreadful electric light that cast false shadows....voices were metallic, without warmth or color. From time to time, a word detached itself from the rest. It repeated itself over and over in my head, absurd, as though cut off by a knife."
- The person may also be flooded by internal stimuli - thoughts and memories. At times these thoughts are experienced as if they have been inserted into the person's head by someone else.
- "a local pharmacist was tormenting me by inserting his thoughts into my head and inducing me to buy things I had no use for."
- While heightened senses are often an early symptom of schizophrenia, the opposite often happens later in its course, and people find their senses blunted (this can include the ability to perceive physical pain - a definite health risk!)
- "However hard I looked it was as if I was looking through a daydream and the mass of detail, such as teh pattern on a carpet, became lost."
- Inability to sort and interpret sensations, and consequently, to respond appropriately
- Normally, the brain sorts through incoming information, interprets it using logic and past experiences, and provides an appropriate (often learned) response. In schizophrenia, this process breaks down
- "If I look at my watch, I see the watchstrap, watch, face, hands, and so on, then I have got to put them together to get it into one piece."
- It can be particularly hard to integrate two different types of stimuli
- "I can't concentrate on television because I can't watch the screen and listen to what is being said at the same time."
- Incoming information is often connected with inappropriate responses - such as laughing when told a loved one has died. Such responses interfere with the ability to relate to other people.
- Thoughts become disorganized or disjointed
- "My thoughts get all jumbled up, I start thinking or talking about something but I never get there."
- The person may also experience periods of thought blocking
- "Sometimes I commit brief disappearances - my mind pauses and closes down for a short while, like falling asleep suddenly"
- Altered sense of self - specifically the sense of where one's body stops and the outside world begins
- The person may experience somatic perceptual distortions
- "Hands, arms, adn legs soemtimes feel an inch to the side of where they really are at. Fingers at times feel and look longer or shorter than usual. My face can feel twice as long as it is."
- They may have difficulty distinguishing themselves from another person, or their reflection
- "several of the patients having breakfast were me. I recognized them by the way they held their knives and forks."
- Different body parts may seem to take on lives of their own
- "The arms and legs are apart and away from me and they go on their own. That's when I feel I am the other person and copy their movements, or else stop and stand like a statue."
- Changes in emotions
- Early in the illness, depression, guilt, fear, exaggerated and rapidly fluxtuating emotions are common
- "I sat in my basement with a fear that I could not control. I was totally afraid - just from watching my cat look out the window."
- Later in the illness, emotions flatten (further hampering relationships by impeding empathy on both sides) - the person may feel "nothing," or they may have emotions but be unable to show them.
- Changes in movement
- Movement may speed up, slow down, and/or become clumsy
- Spontaneity decreases, and repetitive movements may occur
- Some may become catatonic, with the person not moving for an extended period of time
- Changes in behavior
- Other symptoms may cause the person to withdraw and become immobile at times, often to moderate the incoming flood of stimuli.
- Movements are slower due to difficulties with integration
- "If I do something like going for a drink of water, I've got to go over each detail - find cup, walk over, turn tap, fill cup, turn tap off, drink it. I keep building up a picture."
- The person may also engage in ritualistic behaviors - which have a meaning and purpose to the person but seem bizarre to others
- The person may repeat whatever is said to them (echolalia) or mimic behavior (echopraxia)
- Decreased awareness of illness (what we professionals euphemistically call "insight")
- In the early stages of schizophrenia, the person is usually aware that something is going wrong with their brain (which is the most tragic element of the experience, from my perspective). When the disease is fully manifest, however, most lose this awareness as a result of damage to specific parts of the brain.
- Decreased insight results in decreased depression and suicide, but increased involuntary hospitalization and medication refusal.

No comments:
Post a Comment